May-Thurner Syndrome
May-Thurner syndrome, also known as iliac vein compression syndrome, is a condition where the left iliac vein is compressed by the right iliac artery. This vein carries blood from your left leg to your heart. The compression can lead to reduced blood flow in the vein and potentially cause blood clots, a condition known as deep vein thrombosis (DVT).
Symptoms of May-Thurner Syndrome
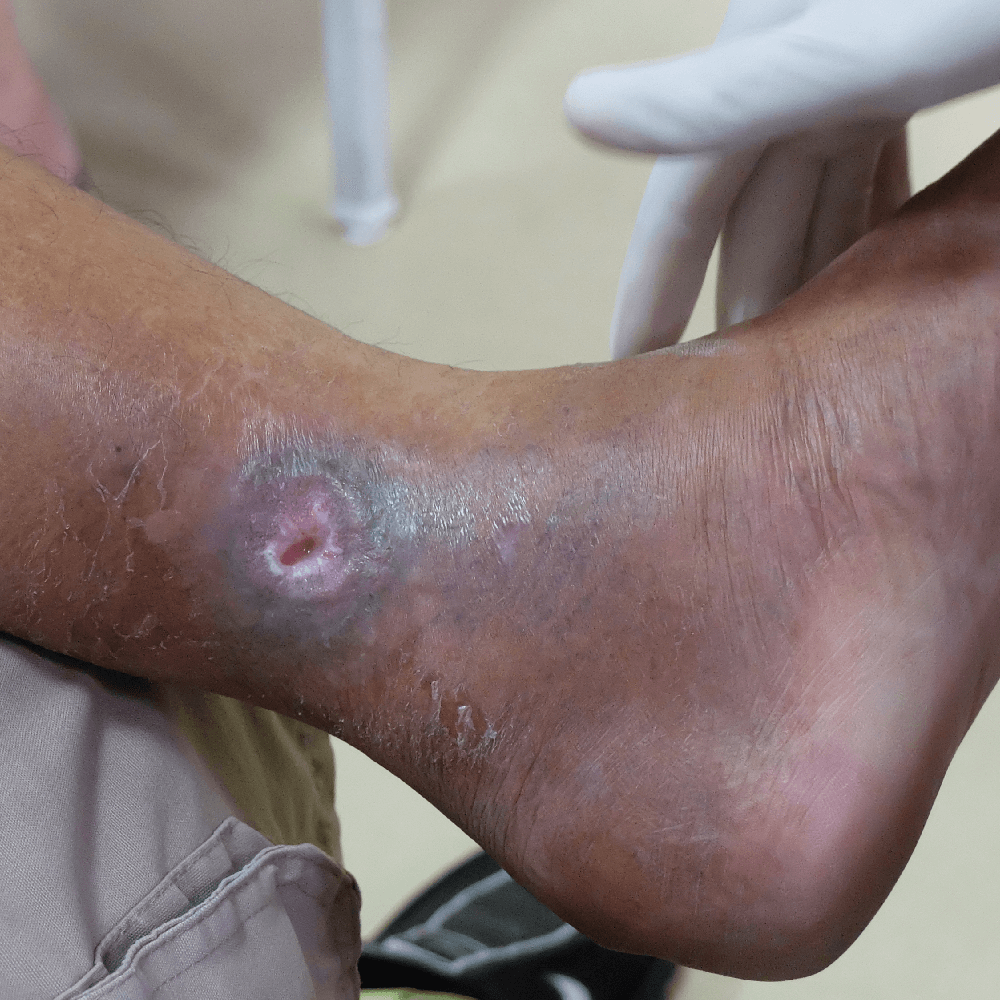
May-Thurner syndrome interrupts typical blood flow through your legs. This can cause blood to pool in your legs, and can develop into deep vein thrombosis. Symptoms will typically only affect the left leg, and may include:
Causes of May-Thurner Syndrome
May-Thurner syndrome is primarily caused by the compression of the left iliac vein by the right iliac artery. Experts aren’t sure why this compression occurs, but some factors can contribute to its development or exacerbate the condition.
Risk Factors for May-Thurner Syndrome
Several risk factors can increase your likelihood of developing May-Thurner syndrome.
The left iliac vein and the right iliac artery are positioned close to each other in the pelvic area. In some individuals, the artery may compress the vein against the pelvic bone, causing the vein to become narrower or obstructed.
Women, especially those who have had multiple pregnancies, are at a higher risk of developing May-Thurner syndrome. Hormonal changes during pregnancy and the pressure exerted on the pelvic veins can contribute to vein compression.
The risk of developing May-Thurner syndrome increases with age.
Sitting or standing for long periods without movement can increase pressure on the pelvic veins. This pressure can contribute to the compression of the left iliac vein by the right iliac artery.
Those with inflammatory conditions or chronic inflammatory disease can contribute to vein inflammation and potentially exacerbate vein compression.
Previous injury or trauma to the pelvic region can lead to changes in vein structure or alignment, making an individual more susceptible to vein compression.
Treatment for May-Thurner Syndrome
May-Thurner syndrome treatment focuses on alleviating the compression of the left iliac vein and restoring proper blood flow. Premier Vein & Vascular offers several minimally invasive procedures for managing May-Thurner syndrome, including:

Angioplasty is a procedure in which a catheter with a small balloon at its tip is used to dilate the narrowed portion of the iliac vein. This helps widen the vein and improve blood flow by relieving the compression.
Learn More

Iliac vein stenting involves inserting a stent into the iliac vein to support its structure and keep it open. This procedure can be highly effective in addressing the compression caused by the adjacent artery and restoring normal blood flow.
Learn More

While primarily used for addressing blood clots, mechanical thrombectomy involves removing or breaking down clots. In the case of May-Thurner syndrome, it could potentially be used to manage severe clotting associated with the condition.
Learn More

FAQs
The compression of the left iliac vein can obstruct blood flow and potentially cause complications, such as deep vein thrombosis, post-thrombotic syndrome following blood clots, venous insufficiency, or pulmonary embolism.
While May-Thurner syndrome is not considered life-threatening, it can lead to serious complications, especially if left untreated or if blood clots develop as a result of the iliac vein compression. The most significant concern associated with the condition is the potential for deep vein thrombosis and subsequent pulmonary embolism, which can be life-threatening.
May-Thurner syndrome is diagnosed through a combination of medical history assessment, physical examination, and imaging tests. Your doctor will start by discussing your medical history, asking about any symptoms you may be experiencing, your overall health, past medical conditions, and family history of vascular or clotting disorders. They will also perform a physical examination, focusing on any signs of swelling, tenderness, discoloration, or varicose veins in the lower extremities. Your doctor may also request imaging tests to assess blood flow and potential vein compression.